 Opioid addiction can begin with the best of intentions, like managing pain. The middle-aged male visits the ER for a back sprain. A typical teenager has her wisdom teeth removed by the oral surgeon. To minimize discomfort, the healthcare professional may prescribe 20 or more hydrocodone pills. In fact, the U.S. Department of Health and Human Services (HHS), estimates that on average, more than 650,000 opioid prescriptions are written and dispensed each day in the U.S.
Opioid addiction can begin with the best of intentions, like managing pain. The middle-aged male visits the ER for a back sprain. A typical teenager has her wisdom teeth removed by the oral surgeon. To minimize discomfort, the healthcare professional may prescribe 20 or more hydrocodone pills. In fact, the U.S. Department of Health and Human Services (HHS), estimates that on average, more than 650,000 opioid prescriptions are written and dispensed each day in the U.S.
Addiction has skyrocketed as a result. The National Institute on Drug Abuse (NIDA) estimates that in 2015, “Two million people in the United States suffered from substance use disorders related to prescription opioid pain medicines and over 33,000 Americans died as a result of an opioid overdose.” NIDA also found that the (negative) impact to the U.S. economy due to prescription opioid misuse to be more than $78 billion a year.
As a result, the Centers for Disease Control (CDC) issued a new guideline in 2016 for the prescription of opioids. Primary-care providers are discouraged from turning to opioids to treat acute pain. The guideline advises doctors to “start low and go slow.” Doctors are urged to prescribe the lowest effective dose in the smallest quantity needed for the time period when pain is severe enough to warrant a narcotic. If an opioid is prescribed, the CDC recommends a faster-acting medication with a short duration of pain relief, rather than slower-acting, extended-release drugs with a longer duration. Adapting to these new guidance may prove challenging for doctors who, throughout their careers, practiced aggressive pain management.
State and the federal government are joining the fight by either evaluating or enacting legislation to limit opioid prescriptions. An article from Bloomberg View reports, “In New Jersey, a patient’s first course of opioids is now limited to five days (30 has been the norm) and the lowest effective dose. A similar bill in the U.S. Senate would limit first prescriptions to seven days. The Senate is also considering taxing prescription opioids to help pay for addiction-treatment services, as are lawmakers in Alaska and California.”
Our country is in the midst of an opioid epidemic. Media attention provides much needed awareness and entities like the CDC deliver education on how to identify, combat, and positively impact the growing issue. Where awareness and education fall short, guidelines and laws aimed at reshaping how physicians address pain management will make the biggest long-term impact. Because of all opioid- related deaths, nearly half of them involve a prescription.
Follow our blog to laern more about opioids and the impact of the opioid abuse.
For information on drug testing, visit our website.
 Your Privacy Choices
|
Privacy Notices
|
Terms
|
Language Assistance / Non-Discrimination Notice | Asistencia de Idiomas / Aviso de no Discriminación | 語言協助 / 不䈚視通知
Your Privacy Choices
|
Privacy Notices
|
Terms
|
Language Assistance / Non-Discrimination Notice | Asistencia de Idiomas / Aviso de no Discriminación | 語言協助 / 不䈚視通知




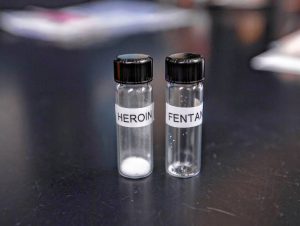













Addiction has skyrocketed as a result. The National Institute on Drug Abuse (NIDA) estimates that in 2015, “Two million people in the United States suffered from substance use disorders related to prescription opioid pain medicines and over 33,000 Americans died as a result of an opioid overdose.” NIDA also found that the (negative) impact to the U.S. economy due to prescription opioid misuse to be more than $78 billion a year.
As a result, the Centers for Disease Control (CDC) issued a new guideline in 2016 for the prescription of opioids. Primary-care providers are discouraged from turning to opioids to treat acute pain. The guideline advises doctors to “start low and go slow.” Doctors are urged to prescribe the lowest effective dose in the smallest quantity needed for the time period when pain is severe enough to warrant a narcotic. If an opioid is prescribed, the CDC recommends a faster-acting medication with a short duration of pain relief, rather than slower-acting, extended-release drugs with a longer duration. Adapting to these new guidance may prove challenging for doctors who, throughout their careers, practiced aggressive pain management.
State and the federal government are joining the fight by either evaluating or enacting legislation to limit opioid prescriptions. An article from Bloomberg View reports, “In New Jersey, a patient’s first course of opioids is now limited to five days (30 has been the norm) and the lowest effective dose. A similar bill in the U.S. Senate would limit first prescriptions to seven days. The Senate is also considering taxing prescription opioids to help pay for addiction-treatment services, as are lawmakers in Alaska and California.”
Our country is in the midst of an opioid epidemic. Media attention provides much needed awareness and entities like the CDC deliver education on how to identify, combat, and positively impact the growing issue. Where awareness and education fall short, guidelines and laws aimed at reshaping how physicians address pain management will make the biggest long-term impact. Because of all opioid- related deaths, nearly half of them involve a prescription.
Follow our blog to laern more about opioids and the impact of the opioid abuse.
For information on drug testing, visit our website.